KCC2 Program
.avif)
FROM ML PRIORITIZATION TO IN VIVO PHENOTYPIC CORRECTION

KCC2 - WHY THIS GENE

KCC2 (SLC12A5) is the principal neuronal chloride exporter that maintains inhibitory GABAergicsignaling. By keeping neuronal chloride low, KCC2 shifts GABA from an excitatory to inhibitorystate. KCC2 hypofunction can drive network hyperexcitability across developmental, rare,acquired, and idiopathic epilepsies.
Approximately 30–40% of epilepsy patients remain drug-resistant, and most current therapiestreat symptoms rather than modify disease. This program focuses on restoring inhibitory circuitfunction with mechanism-linked, quantitative in vivo readouts.
Many epilepsies reflect excitation/inhibition (E/I) imbalance at the circuit level. KCC2 is decision-relevant because it is a direct lever on inhibitory tone via neuronal chloride homeostasis, with atractable path to phenotype-linked validation.
Drug discovery programs can fall short when target hypotheses do not translate into disease-relevant, quantitative in vivo readouts. Our workflow connects target perturbation to seizure-relevant phenotypic correction in a living vertebrate system. We use in vivo perturbation to test whether genetically prioritized signals support a causal contribution to seizure phenotypes,enabling faster target validation.
STEP 1 - PHENOGRAPH™ NOMINATES KCC2 FROM HUMAN EPILEPSY DATA
Discovery stalls when patient signals do not translate cleanly into model readouts. ThePhenograph™ links human clinical phenotypes to model system phenotypes.

- We prioritized epilepsy genes using ML models trained to predict gene-phenotypeassociations.
- We aggregated scores across models to nominate KCC2 (SLC12A5) as a high-priorityepilepsy driver gene
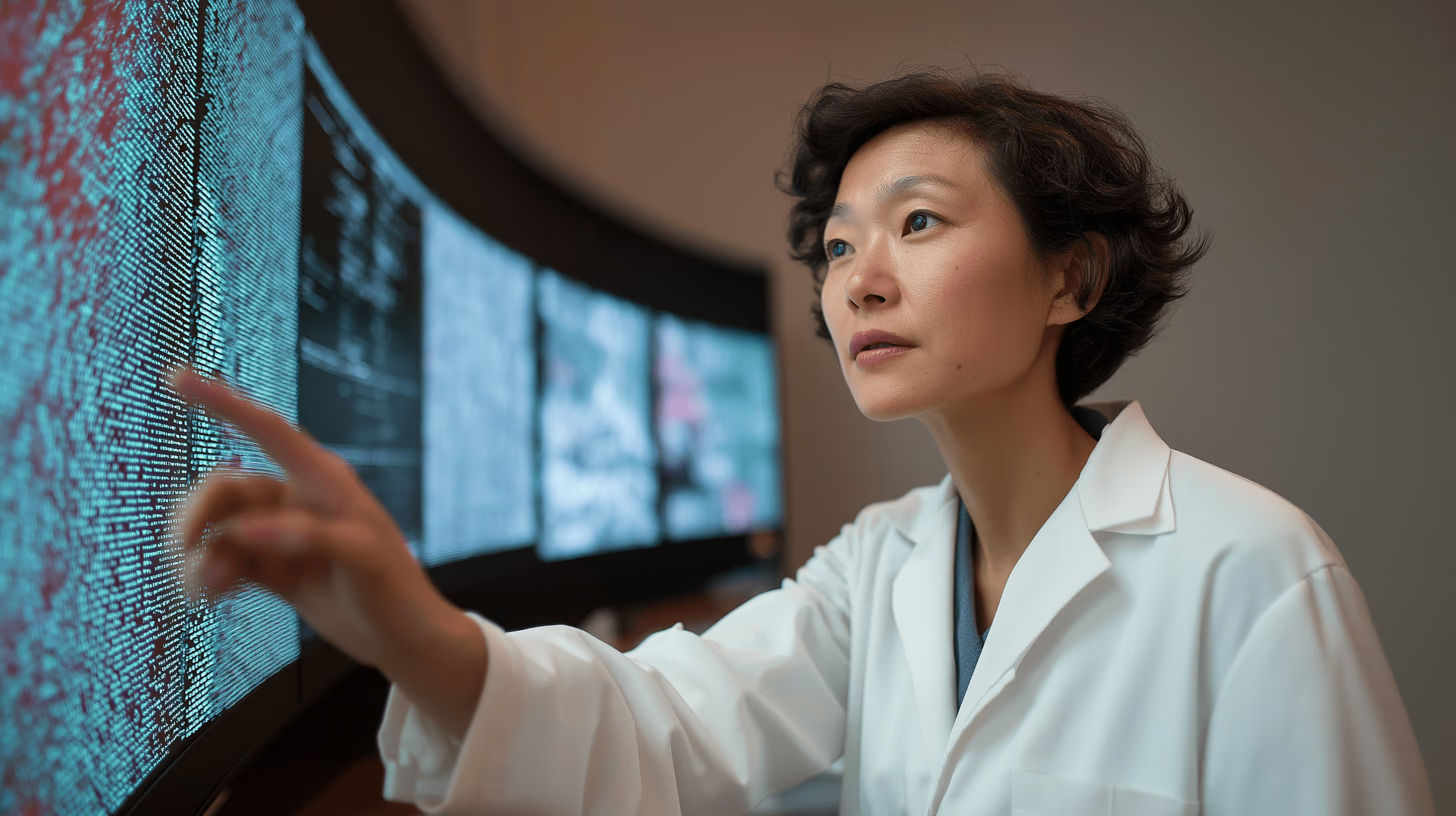

- A target hypothesis grounded in human phenotype, aligned to disease-relevant brain biology,and ready for in vivo validation.


- De-risking target selection by anchoring KCC2 to human epilepsy phenotypes beyondassociation strength alone.
- A clear path to in vivo perturbation and seizure-relevant readouts.

STEP 2 - PHENOMIC ASSAYS BUILD AN IN VIVO KCC2 EPILEPSY MODEL
Target confidence and tractability increase when KCC2 disruption produces a consistent,quantifiable phenotype in a living vertebrate system.

- We developed an in vivo KCC2 epilepsy model.
- We induced KCC2 hypofunction using both genetic and chemical approaches.
- We screened a compound library against the KCC2 hypofunction phenotype.


- KCC2 hypofunction produced a measurable, light-evoked seizure phenotype suitable forscalable screening.
- The chemical model provided higher throughput and a broader sensitivity range for libraryscreening.


- De-risking translation by linking KCC2 hypofunction to a seizure-relevant, quantitative in vivoreadout that supports scalable screening.

STEP 3 - COMPUTER VISION CONFIRMS PHENOTYPIC CORRECTION BY HITCOMPOUNDS
Many screens generate hits. Few produce quantitative evidence of phenotypic correction tied toseizure-relevant readouts.

- We quantified behavioral and morphological responses to support compound detection andprioritization.
- We assessed whether prioritized compounds drive phenotypic correction of the seizurephenotype in vivo.


- A subset of compounds reduced the epilepsy index in the KCC2 models, with effectscomparable to known AEDs.
- Data supported an efficacy signal, evidence consistent with reaching the brain, and noobservable toxicity in this assay context.


- Faster go/no-go decisions by ranking candidate compounds on two questions: whether they correct the seizure-relevant phenotype in vivo, and whether effects are consistent with reaching the brain and being well-tolerated.
- A clearer handoff to downstream development by advancing prioritized compounds withdecision-grade in vivo evidence suitable for lead optimization and partner evaluation.